On June 1, 2020, new age-adjusted telehealth fee codes for visits, counselling and consultations done by phone or video came into effect (see below). While the new fee codes became active on June 1 and the old fee codes inactive, MSP was not able to update Teleplan until late on June 3.
As a result, some EMRs did not update in time for the June 3 MSP cutoff. If you (or your EMR vendor) manually entered the codes, your billings may be rejected. Please check your remittance carefully as you can resubmit rejected billings for the next remittance period.
Contact your EMR vendor or the Teleplan Support Centre for further information.
Download a one page cheat sheet on the Telehealth Fee Codes.
- These new fees have the same value as the in-person fee codes for similar patient encounters.
- These fee codes are for services delivered by phone or video.
- These fee codes should be used regardless of the physician’s location (home, office or Health Authority approved facility).
- Business Cost Premium (BCP) will apply to all of them.
- Retro payments will not be made for dates of service prior to June 1, 2020.
- From March 16 – May 31, 2020, the same telehealth fee codes for visits, counselling and consultations done by phone or video are to be used for patients, regardless of age. (13037 and 13038 in most circumstances). From June 1 onwards, use the new fee codes for phone and video services.
Please visit our COVID-19 billing page for more billing information related to COVID-19.
Full information about all the fees that can be billed for Virtual Care (Telehealth) can be found in the Simplified Fee Guide (member-benefit). You can read more about becoming a member here.
Effective June 1, 2020
Download a one page cheat sheet on the Telehealth Fee Codes
These fees cannot be correctly interpreted without reference to the Preamble D.1 in the MSC Payment Schedule.
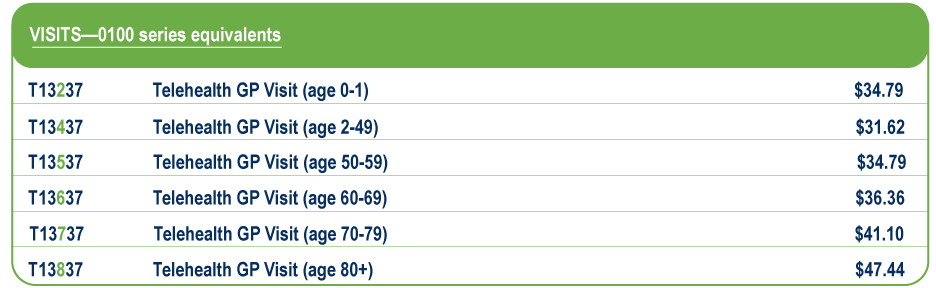
Bill the following codes for a Telehealth Visit (0100-series equivalent), regardless of your location (home, office or Health Authority approved facility).
**Submission of fee codes 13037 and 13017 with dates of service on or after June 1 will be rejected.
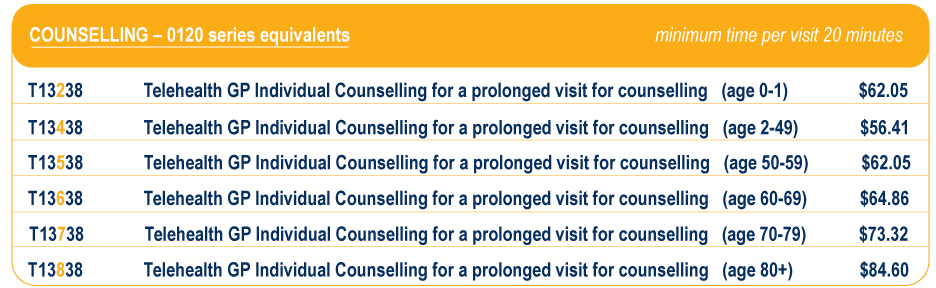
Bill the following codes for Telehealth Counselling (0120-series equivalent), regardless of your location (home, office or Health Authority approved facility).
**Submission of fee codes 13038 and 13018 with dates of service on or after June 1 will be rejected.
Notes:
i ) MSP will pay for up to four (4) individual counselling visits (any combination of age appropriate in office, out of office, and telehealth) per patient per year (see Preamble D. 3. 3.)
ii) Start and end time must be entered into both the billing claims and patient’s chart.
iii) Documentation of the effect(s) of the condition on the patient and what advice or service was provided is required.
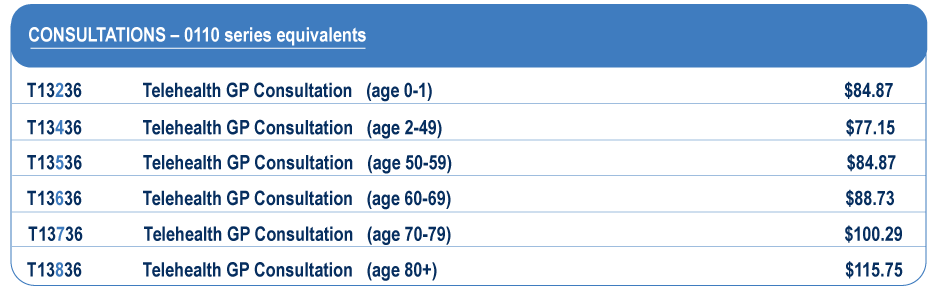
Bill the following codes for Telehealth Consultations (0110-series equivalent), regardless of your location (home, office or Health Authority approved facility).
**Submission of fee codes 13036 and 13016 with dates of service on or after June 1 will be rejected .
Non-procedural interventions where there is no telehealth fee may be claimed under the face-to-face fee with a claim note record that the service was provided via telehealth.
- Examples include Palliative Care Facility visits (00127), Management of Maintenance Opioid Agonist Treatment (00039), and Group Medical Visits.
- You can read more information about how to bill for LTC Facility visits (00114) here.
Prior to June 1, 2020
These fees cannot be correctly interpreted without reference to the Preamble D.1. in the MSC Payment Schedule.
If you are physically located in your clinic/home or other location (that is not a Health Authority facility) when calling your patient:
Bill 13037 for the equivalent of an in-office visit (00100, 12100, 15300, 16100, 17100, 18100):
13037 Telehealth GP in-office Visit ………………………………………………………………………$34.44
Bill 13038 for a counselling visit (instead of 00120, 12120, 15320, 16120, 17120, 18120):
13038 Telehealth GP in-office Individual counselling for a prolonged visit for counselling (minimum time per visit – 20 minutes)………………………………………………$58.90
Notes:
i ) MSP will pay for up to four (4) individual counselling visits (any combination of age appropriate in office, out of office, and telehealth 13018 and 13038) per patient per year (see Preamble D. 3. 3.)
ii) Start and end time must be entered into both the billing claims and patient’s chart.
iii) Documentation of the effect(s) of the condition on the patient and what advice or service was provided is required.
If you are physically located in a Health Authority facility when calling your patient:
For the billing of the GP Telehealth out-of-office fees 13016, 13017, 13018, 13021 and 13022, out-of-office shall mean that the physician providing the service is physically present in a Health Authority approved facility. The name of the facility and the results of the Telehealth service must be recorded in the patient chart.
Bill 13017 for an out-of-office visit:
13017 Telehealth GP out-of-office Visit…………………………………………………………………$41.10
Bill 13018 for an out-of-office counselling visit:
13018 Telehealth GP out-of-office Individual counselling for a prolonged visit for counselling (minimum time per visit – 20 minutes)………………………………………..$75.32
Notes:
i) MSP will pay for up to four (4) individual counselling visits (any combination of age appropriate in office, out of office, and telehealth 13018 and 13038) per patient per year (see Preamble D. 3. 3.)
ii) Start and end time must be entered into both the billing claims and patient’s chart.
iii) Documentation of the effect(s) of the condition on the patient and what advice or service was provided is required.
If you are doing consultations by referral, the following fee codes apply:
Bill 13036 for a consultation done when you are physically located in your clinic/home or other location (that is not a Health Authority facility) :
13036 Telehealth GP in-office Consultation…………………………………………………………..$82.43
Bill 13016 for an out-of-office consultation done when you are physically located in a Health Authority facility:
13016 Telehealth GP out-of-office Consultation …………………………………………………..$109.02
What is a consultation?
GP Consultations apply when a medical practitioner (GP or Specialist), or a health care practitioner (midwife, for obstetrical or neonatal related consultations; nurse practitioner; oral/dental surgeon, for diseases of mastication), in the light of his/her professional knowledge of the patient and because of the complexity, obscurity or seriousness of the case, requests the opinion of a general practitioner competent to give advice in this field. A consultation must not be claimed unless it was specifically requested by the attending practitioner.
The service consists of the initial services of GP consultant, including a history and physical examination, review of x-rays and laboratory findings, necessary to enable him/her to prepare and render a written report, including his/her findings, opinions and recommendations, to the referring practitioner. Consultations will not apply if the referred patient has been attended by the consulting general practitioner or another general practitioner in the same group during the preceding six months.”

