
LFP Payment Model: Inpatient Care
The content of this page is available to Members of BC Family Doctors.
Members, please log in. Non-members, please Click here for details on how to join.

Will more doctors solve access to primary care?
…ding longitudinal care because of heavy administrative burdens and better compensated opportunities in other areas of care. Patient needs have changed as well. There are increasing healthcare needs from an aging population as well as a rising need for mental health care in younger people. Read the full article here….

Congrats to PEI on new agreement with family doctors!
…PEI announced a new agreement with physicians, designed to improve primary healthcare recruitment and retention. Key highlights of the new agreement include: Recognizing family medicine as a specialty; Improving compensation for family physicians in PEI; Creating a new incentive for family physicians who care for a patient panel above their expected amount; Increasing compensation across the board for all specialists; and Reducing red tape and adm…

Sharing family doctor advice for flu season
…yourself against the flu. Family doctors play a critical role during respiratory illness season, helping patients navigate flu season with comprehensive health advice, immunizations, and preventive healthcare. Dr. Zeineddin shared the best ways to stay healthy this flu season, including getting a flu shot and caring for yourself. Watch Dr. Zeineddin’s interview here!…

B.C. has more family doctors with new payment model, but issues still need addressing
…gh-functioning, well-funded family medical clinics are the backbone of our health system, but the old family doctor payment model made this impossible to achieve. B.C.’s new family doctor payment model has kept me in the game. The new Longitudinal Family Physician (LFP) Payment Model, introduced February 2023, makes things much simpler. I’m not spending as much time on billing and my staff don’t have to keep track of countless billing codes. No…

Your doctor won’t see you—why the LFP Payment Model matters
…time and effort needed to manage patients with chronic conditions, mental health needs and other complex issues. For many, fee-for-service billing made family medicine unsustainable. The Longitudinal Family Physician (LFP) Payment Model, introduced in B.C. almost two years ago, is a step in the right direction. By compensating doctors for time spent providing comprehensive, patient-centred care, the LFP model allows doctors to focus on building r…

The importance of having a family doctor
…family doctor, everyone loses. Patients without a family doctor face worse health outcomes—more hospitalizations, higher mortality rates and fragmented care. For the healthcare system, the impact is just as serious, with increased costs and inefficiencies straining limited resources. The reasons behind the crisis are no surprise: an aging workforce, fewer graduates choosing family medicine and the unsustainable pressures of the job. Here in B.C.,…
Make an impact: join our board and committees!
…imary care change. Use your voice to represent your colleagues and improve health care in British Columbia. We need a range of voices from different demographics, geographies and viewpoints to drive primary care change. We’re currently looking for members for the following roles: Board District Delegate Positions We have two vacant Board positions we need to fill. You must reside in the district to be eligible. Terms are from February 2025 to Ju…

Why paperwork is driving doctors away—and how to fix it
…rative stress is a key element to keeping doctors in practice. The Colwood Health Clinic on Vancouver Island is showing one way that it can be done. The clinic introduced a team-based care model. Under the new Colwood model, the city employs doctors directly, providing pension and benefits—and takes on some of the paperwork associated with running a family medicine clinic. This approach makes the job more rewarding for doctors by ensuring patient…
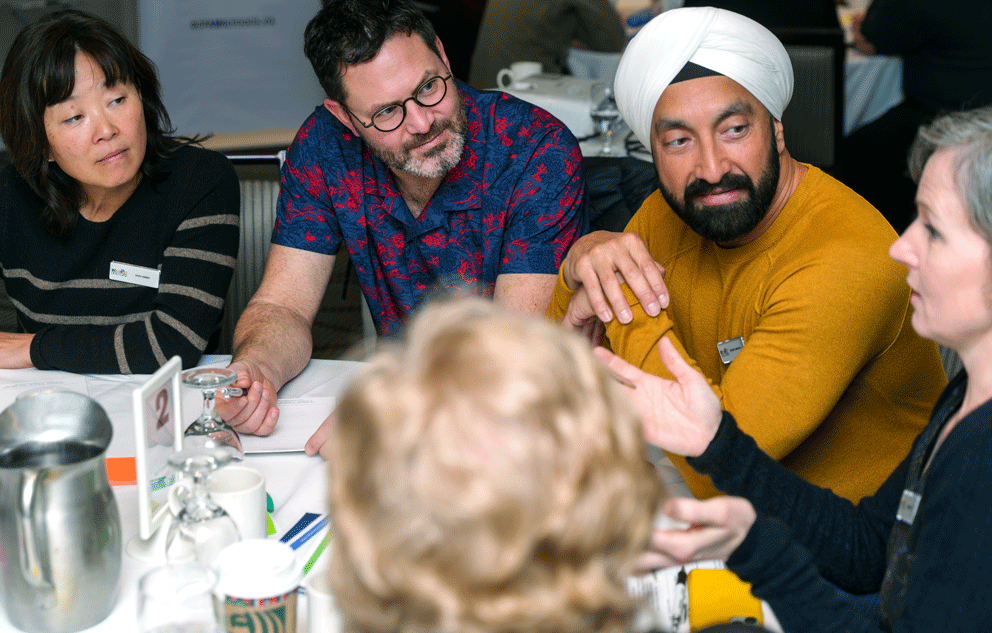
Amplifying patient voices in primary care
…t OurCare Report shed light on the challenges and opportunities facing our health care system and what Canadians said they need from primary care. 📖 Read the report to learn about the OurCare Standard. 📽️ Watch the video to hear real stories and insights from patients. 📊 Stay tuned! A new survey launches in February to give patients in British Columbia a chance to share their experiences and see how they match up to the OurCare Standard. Your voic…

Dr. Darren Joneson on mental well-being & healthcare reform
…President-Elect Dr. Darren Joneson recently joined the Your Health Care Matters podcast for a thoughtful discussion on the challenges facing B.C.’s healthcare today. From self-compassion and mental well-being to incentivizing the right things in primary care, this conversation explores how we can build a stronger, more sustainable system where physicians and patients can thrive. 🎧 Watch now https://www.youtube.com/watch?v=na4lDlr7nZs…

Family doctors and specialists: Working together for better patient care
…ncreasing and patients are feeling the impact. That’s why we’ve written to Health Minister Josie Osborne to highlight the growing challenge of specialist wait times. We’re calling for stronger referral systems, better coordination between family doctors and specialists and the right resources to support patients while they wait. Family doctors are the foundation of our healthcare system. Strengthening access to care means better outcomes for patie…

A race against time: How virtual supports helped save a life in rural B.C.
…a video call away, the team stabilized the patient and arranged for life-saving treatment. This is what Fair Care Everywhere is all about. No British Columbian should face barriers to care just because of their postal code. Family doctors are at the heart of our health care system, but they need the right support, resources and system-wide commitment to provide care—no matter where their patients live. Fair Care Everywhere means ensuring no one is…

Strengthening family medicine together: An update from Maryam
…e models which aim to enhance access, alleviate your workload and create a healthcare system where both doctors and patients can flourish. Reducing administrative burdens The struggle with excessive paperwork and sick notes is a significant issue. We have raised this with Health Minister Josie Osborne and are hopeful reforms will be implemented to reduce these burdens soon including eliminating sick notes. Advocating for policy improvements Family…

New Fee: Management of Stillbirth
The content of this page is available to Members of BC Family Doctors.
Members, please log in. Non-members, please Click here for details on how to join.

Fee-For-Service: Long-Term Care Updates
The content of this page is available to Members of BC Family Doctors.
Members, please log in. Non-members, please Click here for details on how to join.

The heart of family medicine: Trust, tragedy and the bonds that endure
…me beyond Canada. I’ve practiced in Guatemala and Africa, where access to healthcare is limited and the role of a family doctor is vital. Mentoring the next generation of doctors I work in a learning centre where we train residents so we’re one of the few clinics still taking new patients. You really get a sense of how conditions and health concerns are neglected without access to primary care – it’s a major challenge. Specialist access is also a…

What family doctors need from the 2025 provincial budget
…’t do it alone. We need a healthcare system that integrates nurses, allied health professionals and administrative support into family practice clinics. A funded, coordinated team-based care model would allow doctors to focus on what they do best—caring for patients—while ensuring that everyone gets the care they need. 3. Administrative reform to reduce paperwork Family doctors spend too much time on paperwork and not enough time with patients. Th…

Beyond the clinic: The reality of rural family medicine
…ugh people to meet the demand. On top of that, we don’t have enough allied health support. We have almost no social workers, no outpatient physiotherapy. If you break a leg, I have to teach you how to use crutches. If you have surgery in an urban centre, I have to manage your follow-up care because the specialists expect it. In rural medicine, you’re not just a doctor. You’re also a counselor, a rehab specialist, an advocate. The workload is enorm…

It takes a village: Why we need team-based care
…, separate from physician pay. These clinics wouldn’t be government-run or health authority-controlled. Instead, they would be operated by non-profit boards, ensuring community-focused care that isn’t dependent on individual doctors. This model would provide stable funding for nurses, dietitians, physiotherapists, counselors, and other key team members, so care doesn’t fall apart when a doctor retires or leaves. Another project I’m working on is a…
