The Future of Virtual Care
Guiding Principles for a Connected Future
In just five years, virtual care in BC has grown from an emergency stopgap to a vital part of healthcare. To build a modern health system, we must thoughtfully integrate virtual and in-person care – ensuring access, equity, safety, and quality for all British Columbians.
WHAT IS VIRTUAL CARE?
Any interaction between patients and their circle of care that occurs remotely using any forms of communication or information technologies.
Our Five Guiding Principles
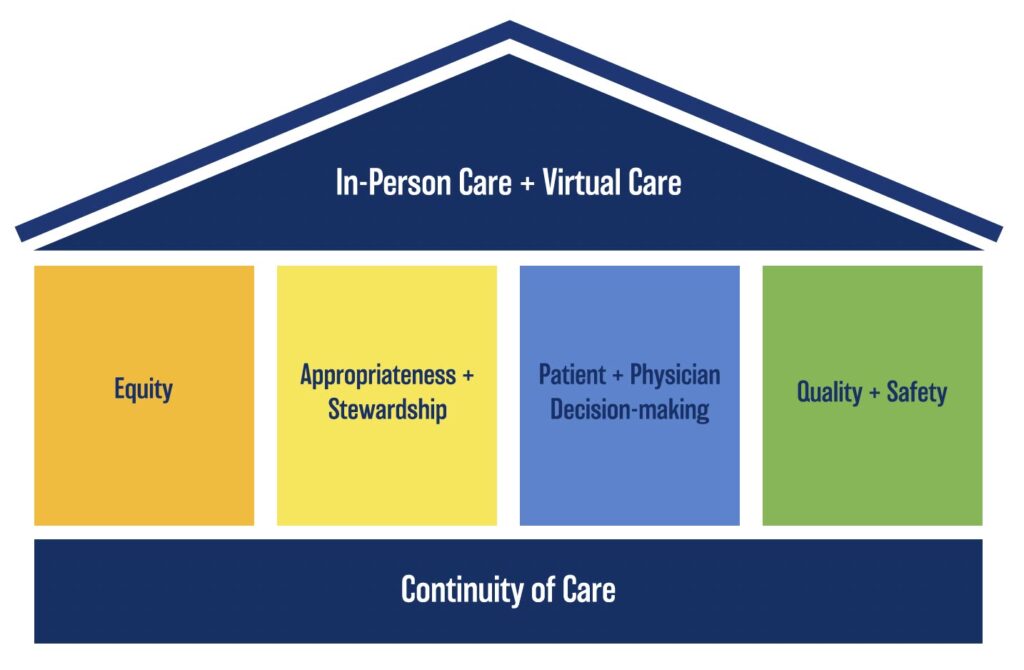
1. Continuity of Care
Continuity of care is foundational to virtual care provision. Virtual care is most effective when delivered within a patient-physician relationship that incorporates relational, informational, and management continuity. These aspects of continuity of care are a key element of many types of family medicine care. While virtual care can be appropriately used in episodic care, it works best when patients also have access to ongoing and in-person services.
2. Equity
Healthcare services—both virtual and in-person—must be designed and delivered with an equity-first approach. We must recognize the diverse needs and digital literacies of patients and communities. This means supporting virtual care provided by both video and phone, since many British Columbians lack reliable high-speed internet. The goal is to create equity-driven virtual care policies that remove barriers for underserved and marginalized communities.
3. Appropriateness & Stewardship
Clinically appropriate care depends on various considerations, including the need for a physical examination and the patient’s unique clinical, social, and cultural needs. At the system level, we have a collective obligation to protect and strengthen BC’s publicly funded healthcare system by prioritizing the accountable integration of virtual care within physician-operated clinics, health authorities, and non-profit organizations.
4. Patient & Physician Decision-Making
Healthcare decisions are complex and deeply personal. We support shared decision-making, with patients and physicians choosing the care modality together. Equal compensation for in-person and virtual care ensures that patient needs—not compensation structures—drive decisions about care delivery.
5. Quality & Safety
Patients deserve safe, high-quality care whether it’s delivered in-person or virtually. Experience from integrated health systems suggests that at least 50 percent of care can be safely delivered by phone, video, and secure email when provided in an integrated, team-based care model. Primary care improvements and virtual care integration must be pursued and evaluated together as essential drivers of quality and safety.
Our Recommendations for Virtual Care Compensation
To strengthen patient care during this time of healthcare transformation, we recommend five concrete measures:
- Use an equity-first approach when designing physician compensation for in-person and virtual care.
- Provide equal compensation for physician care provided virtually or in-person.
- Expand team-based care by funding virtual services that are delegated to other healthcare professionals with appropriate scope of practice.
- Invest in physician education about delivering a balance of virtual and in-person care appropriate to their patient population and community context, without limiting virtual care visits.
- Incorporate payment for asynchronous care modalities, such as secure messaging, remote monitoring, and other evidence-based virtual modalities.
Building a Connected Future
Virtual care is essential to building a modern healthcare system that meets the needs of today’s patients and tomorrow’s healthcare challenges. Now is the time to act – let’s create a bold, connected, and equitable future for healthcare in British Columbia.